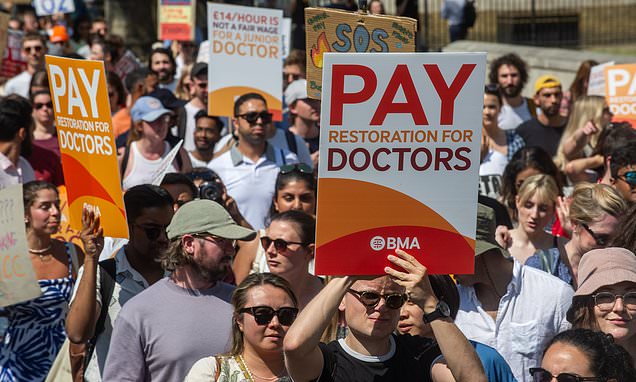
Downing Street blasts senior doctors for planning to put ‘profits before patients’ by carrying on with lucrative private work while on strike
- PM spokesman said it ‘cannot be right’ for doctors to practice privately on strike
Downing Street has blasted hospital consultants planning to put ‘profit before patients’ by carrying on with their lucrative private work while on strike.
The Prime Minister’s spokesman said it ‘cannot be right’ that senior doctors continue to treat their fee-paying patients at the same time as NHS procedures are cancelled during next month’s two-day walkout.
No10 spoke out yesterday after it was revealed that the wealthy medics, who earn £128,000 on average for their public sector work, are allowed by their union to continue in private practice even when they are taking industrial action.
Asked what Rishi Sunak made of their behaviour, the PM’s official spokesman replied: ‘If consultants choose to take strike action, it cannot be right that some continue to only treat their fee-paying private patients and benefit financially from that while patient care is put at risk in the NHS.
‘We would urge those consultants considering this approach to seriously consider the impact on the NHS. It would not be right to put profit before patients.’
Downing Street has blasted hospital consultants planning to put ‘profit before patients’ by carrying on with their lucrative private work while on strike
Up to 24,000 hospital consultants are due to strike on July 20 and 21, for the first time in more than a decade, claiming their incomes have fallen by 35 per cent in the past 15 years.
They will provide ‘Christmas Day cover’, meaning that routine operations will be cancelled but life-or-death services in A&E and maternity will remain in place.
The action has been timed to start the day after junior doctors in England complete a five-day walkout, adding to the disruption suffered by patients.
It comes after the head of the British Medical Association warned that all four types of doctors could be in dispute with the Government ahead of the next election.
Professor Philip Banfield said GPs and specialist doctors may join in the rows over pay and conditions. Specialists say the value of their pay has fallen by 25 per cent since 2008 while GPs are angry about a new contract being imposed on them.
‘What you could have is a situation where junior doctors, consultants, specialist and speciality doctors, and GPs are all in dispute with the Government in the run-up to a general election,’ Professor Banfield told The Guardian. ‘That is what we are planning for.’
Industrial action across the NHS risks the PM’s key pledge to cut waiting lists, with a record 7.4million patients now waiting to start hospital treatment.
Dissatisfaction over pay in the health service has continued alongside poor mental health among staff.
Dissatisfaction over pay in the health service has continued alongside poor mental health among staff
Figures show that burnout and other mental health issues have remained the main cause of sick days. Data from NHS Digital shows 24.6 per cent of staff sickness absences in NHS England were down to anxiety, stress, depression and other psychiatric illnesses in February.
The overall absence rate that month was 5 per cent, down from 5.3 per cent in January and 6.3 per cent in December.
Separate analysis from the Nuffield Trust think-tank found that the average rate of sickness absences in NHS England in 2022 was 5.6 per cent, compared with 4.3 per cent in 2019, the year before the pandemic.
The researchers claim this equates to the loss of 75,000 staff, an increase of 29 per cent over three years.
It said ambulance staff, ambulance support staff and midwives had the largest rises in sick days in 2022 compared with 2019.
Dr Billy Palmer, a senior fellow at the Nuffield Trust, said: ‘The increasing numbers taking time away from work feeds into a seemingly unsustainable cycle of increased work leading to burnout and then more people choosing to leave.
‘There has been a lot of focus on recruitment… but we need more endeavour to improve the working conditions of existing staff and protect them from illness.’
NHS ‘has culture of cover-ups and lies over needless deaths’
The NHS is beset with a ‘culture of cover-up’ and ‘defensiveness’ when patients are avoidably harmed, a damning report has concluded.
Hospitals ‘routinely’ fail to accept their errors and often withhold information from families who have needlessly lost loved ones, according to the country’s health ombudsman.
Rob Behrens said he had seen evidence of patients being lied to and records altered after their death to cover up mistakes.
He said such cover-ups must be challenged and accountability ‘has to be at all levels’, adding ‘the minister has to be accountable and NHS England has to be accountable’.
He told a briefing: ‘There is a culture of cover-up. Patients have been lied to, their care plans altered after they died, and there are a whole series of incidents where people do not know what went on and hospitals are reluctant to disclose this. You can call it what you like but it is a cover-up.’
His team examined 22 cases of avoidable death and concluded there were four main causes of harm – failure to make the right diagnosis, treatment delays, poor communication between staff and a failure to listen to the concerns of patients or their families. For most of the deaths probed by the ombudsman, the trust involved had not conducted a serious incident investigation.
The report referenced a baby who died when antibiotics were not given soon enough. It said details were not given to his parents for seven weeks and ‘staff discussed deleting a recording made during a meeting when the parents stepped out of the room, because they realised what they had said might get the trust into difficulty’.
NHS figures suggest there are an estimated 11,000 avoidable deaths every year due to patient safety failings.
In a foreword to the report, Mr Behrens said ‘one of the biggest threats to saving lives is a healthcare system at breaking point’, adding: ‘The Government says patient safety is a priority but if it means this, the NHS must be given the workforce capacity it needs.’
Source: Read Full Article